IUD

IUD: what is it and how does it work?
The intrauterine device is one of the most reliable methods of long-acting contraception; it’s a small flexible device that the doctor installs directly into the uterus. The procedure takes only a few minutes, and the effect lasts for several years, depending on the type of IUD.
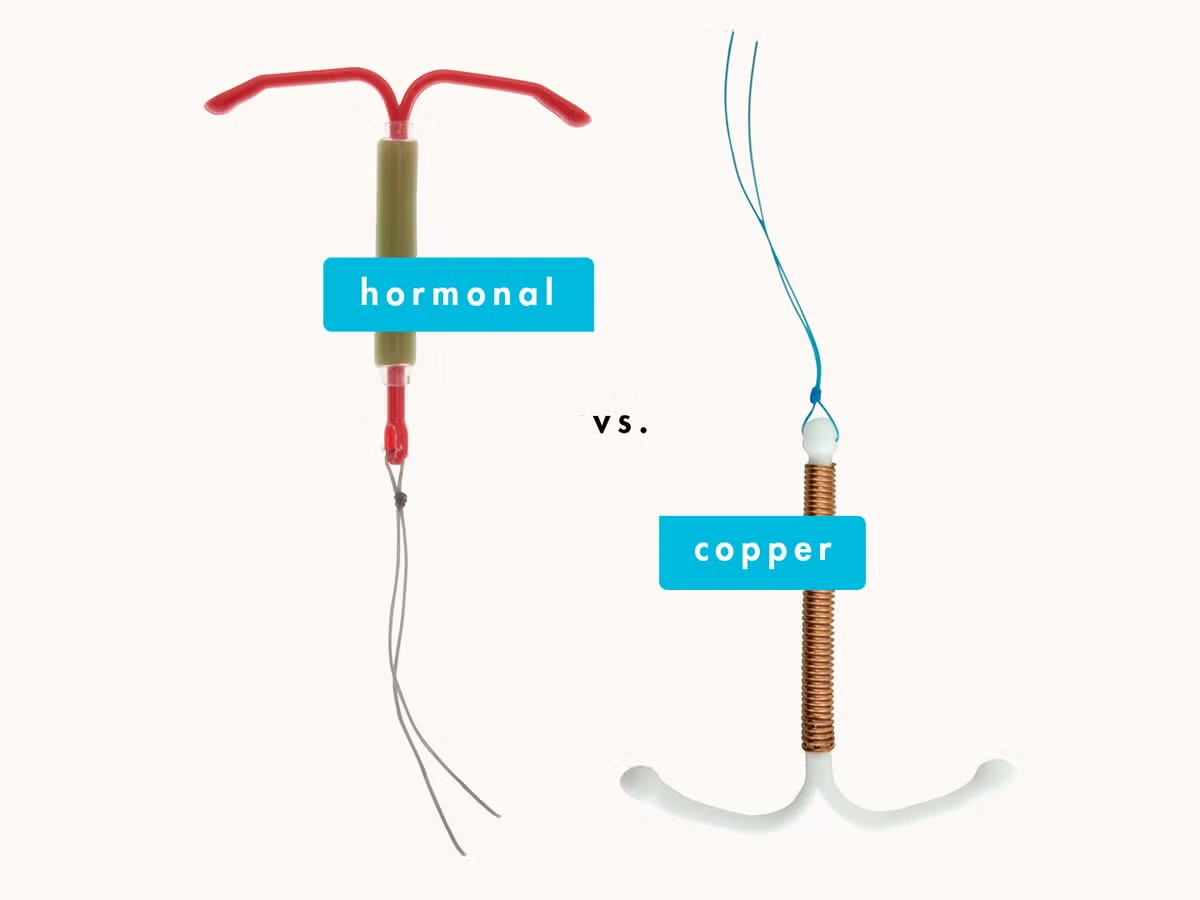
There are two main types of IUDs. The first is the copper IUD, which releases copper ions, creating an unfavorable environment for sperm and preventing them from reaching the egg. The second type is the hormonal IUD, which gradually releases hormones, thickening the mucus in the cervix and preventing fertilization.
Both options effectively protect against unwanted pregnancy, but the choice of the appropriate model depends on the individual characteristics of the body and the doctor's recommendations.
What are the different types of IUDs and how do they work?
There are two main types of intrauterine devices on the market today - copper (inert) and hormonal. They differ in their mechanism of action, but both are effective in preventing pregnancy, providing long-term protection.
- The copper IUD is T-shaped and covered with a thin copper wire. It releases copper ions that create an unfavorable environment for sperm, reducing their motility and fertility. Copper has also been proven to have a spermicidal effect, making the method even more reliable. In this sense, this option is ideal for women who are not suited to hormonal contraceptives and begin working immediately after insertion.
- The hormonal IUD gradually releases small doses of hormones that prevent pregnancy in two ways. First, the hormones thicken the mucus in the cervix, preventing sperm from reaching the egg; second, they suppress ovulation, preventing the egg from leaving the ovary. An added benefit is that hormonal IUDs can reduce painful or heavy menstruation. However, unlike the copper IUD, they do not start working immediately, but about a week after insertion.
The choice between these options depends on the individual characteristics of the body, and the final decision is made by the doctor after consultation. Both types of spirals can be worn for a long time, and if desired, they can be removed at any time if a woman is planning a pregnancy.

Why choose a copper intrauterine device?
Copper IUDs are one of the most reliable and convenient methods of contraception, which are popular among women due to their effectiveness and long life. They do not require daily monitoring, are suitable for most women and have several significant advantages.
One of the major pluses is that they are highly effective - over 99% effective; this means that the chance of pregnancy is virtually none when used correctly. In addition, copper spirals last up to 10 years, which makes them one of the most durable methods of contraception.
Another important factor is cost-effectiveness., since unlike pills or injections which require regular purchases, the IUD is inserted once and does not require frequent medical checkups.
Also, copper spirals do not contain hormones, so they do not cause side effects associated with hormonal contraception. They do not affect the natural processes in the body, do not reduce fertility - after their removal, the ability to conceive is restored almost immediately. In addition, studies show that IUDs can reduce the risk of cervical and ovarian cancer. They can even be used as emergency contraception if insertion occurs within 5 days after unprotected intercourse.
Another convenience - intrauterine devices do not interfere with intimate life. They are compact, inside the uterus and are not felt during sex. They can be inserted immediately after childbirth, cesarean section or abortion, which makes this method accessible and convenient for women in different situations.
Possible side effects and disadvantages of the IUD
Although the IUD is a convenient and effective method of contraception, it is worth considering the possible disadvantages and side effects before inserting it.
First of all, the intrauterine device does not protect against sexually transmitted infections; the only way to avoid such diseases is to use barrier methods of contraception, such as condoms. Moreover, in some cases, the IUD can even increase the risk of inflammation, which makes it not the best option for women who change partners frequently.
Another point is the discomfort of insertion and removal. The procedure takes only a few minutes, but may be accompanied by discomfort or mild pain, especially if a woman has not given birth before.
Although the likelihood of pregnancy when using the IUD is extremely low, if it does occur, there is an increased risk of ectopic pregnancy. Therefore, it is important to have regular checkups with a gynecologist to monitor the position of the device.
Some women may experience irregular bleeding and cramping in the first few months after insertion, especially if a hormonal IUD is used. Usually, these symptoms go away after 3-4 months as the body adapts.
Another disadvantage is the need to see a doctor for insertion and removal, since unlike pills or condoms, an IUD cannot just be taken and used on its own. In addition, in rare cases, the IUD can accidentally dislodge or fall out, and in exceptional situations, it can even damage the uterine wall, which requires its immediate removal.
How is an IUD inserted and removed?
IUD insertion and removal is a medical procedure that must be performed by a gynecologist in a clinic or office. Before installation, the specialist will explain how everything will go and answer the patient's questions.
How does the installation take place?
The woman is placed on the gynecological chair, as in a normal examination. The doctor checks for inflammation or infection, then uses a gynecologic mirror (speculum) to dilate the vagina and examine the cervix.
The IUD is inserted into the uterus with a special applicator, after which the doctor carefully removes the applicator, trims the IUD threads (they remain in the cervical canal) and removes the speculum. The procedure takes a few minutes, but may be accompanied by discomfort or cramps, especially in women that have not given birth.
How is the removal process?
The process of removing the IUD is very similar, but instead of an applicator, the doctor uses forceps. Grasping the threads of the spiral, the doctor gently pulls on them, and the device easily comes out. At this point, the woman may feel a brief spasm, but in most cases the procedure is quick and painless.
Before insertion or removal, you can take an analgesic to reduce discomfort. It is important to remember that after removal of the IUD, fertility is restored almost immediately, so if a woman is not planning a pregnancy, she should immediately take care of other contraception.

FAQ`s
Who should not have an intrauterine device?
The IUD is contraindicated in women with unexplained menstrual irregularities, endometriosis, uterine adhesions and anatomical abnormalities.The IUD should not be used in case of sexually transmitted infections, cervical cancer and pregnancy.
How do I feel after IUD insertion?
After IUD insertion, women often experience mild cramping, pulling pains in the lower abdomen or discomfort in the lower back; as there may also be some bleeding, which usually subsides after a few days.It takes time for the body to get used to the spiral, so there may be irregular discharge or increased menstrual pain in the first few weeks. This is a normal reaction, but if the discomfort becomes too severe or lasts longer than a few weeks, you should consult your doctor.
When should I worry after IUD insertion?
It is normal to experience some discomfort after insertion, but if you experience severe cramping, heavy bleeding or fever, it may indicate complications.These symptoms may indicate a misplaced IUD, inflammation or infection, so you should see your doctor immediately if you experience them. Severe pain or prolonged discomfort should not be ignored, as the IUD should provide comfortable protection and not cause serious discomfort.
Do I need to see a doctor after IUD insertion?
After insertion of the IUD, it is recommended to come for a check-up after 2-4 weeks to make sure that the IUD is in the correct position.If there is no discomfort, regular visits are not required - a second examination is only necessary if there is pain, unusual discharge or suspicion of displacement of the IUD. However, in case of any doubts, it is better to consult a doctor to avoid possible complications.
How much does an IUD cost?
The price of an IUD depends on the country and the type of device. On average, the cost ranges from $35 to $100, but in some regions the IUD may be provided free of charge as part of government programs or health insurance.It is also worth considering additional costs , such as gynecologist consultation, installation and follow-up examinations, which can affect the final cost of the procedure. It is better to clarify the details in advance at the medical institution where the installation is planned.

Posts:
Photos/Videos:
/

Posts:
Photos/Videos:
/

Posts:
Photos/Videos:
/

Posts:
Photos/Videos:
/